Here’s a detailed, unique article titled “Headaches: Causes, Treatments, and Prevention Strategies” with a clear step-by-step guide to writing a similar article from scratch.
Headaches: Causes, Treatments, and Prevention Strategies
Headaches are among the most common medical complaints worldwide. Affecting people of all ages, they can vary significantly in intensity, duration, and underlying cause. While some headaches are minor and occasional, others can be chronic and debilitating, significantly affecting quality of life. Understanding the root causes, available treatments, and effective prevention methods is essential for managing and minimizing the impact of headaches.
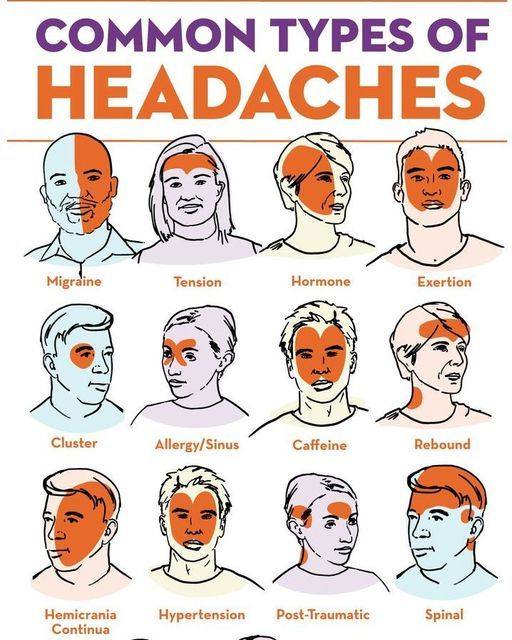
1. Types and Causes of Headaches
Headaches are generally categorized into two broad groups: primary and secondary headaches.
Primary Headaches
These are not symptoms of an underlying illness. They include:
Tension Headaches: Caused by muscle tension, stress, or poor posture. They are the most common type and typically result in mild to moderate pain.
Migraine Headaches: Characterized by intense, throbbing pain, often accompanied by nausea, vomiting, and sensitivity to light or sound.
Cluster Headaches: Severe, one-sided headaches that occur in cyclical patterns or clusters. These are less common but extremely painful.
Secondary Headaches
These result from underlying health conditions, such as:
Sinus infections
High blood pressure
Head injury
Medication overuse
Tumors or neurological disorders
Identifying whether a headache is primary or secondary is crucial for appropriate treatment.
2. Common Triggers
Recognizing triggers can help in avoiding or minimizing headache episodes. Common triggers include:
Stress and anxiety
Sleep disturbances
Dehydration
Skipping meals
Caffeine withdrawal
Bright lights or loud noises
Hormonal changes (especially in women)
Keeping a headache diary can be useful in identifying personal triggers.
3. Treatment Options
Treatment strategies vary based on the type and severity of the headache.
A. Medication
Over-the-counter (OTC): Ibuprofen, aspirin, acetaminophen for mild headaches.
Prescription medications: Triptans and ergotamines for migraines.
Preventive medications: Beta-blockers, antidepressants, or anticonvulsants for chronic headaches.
B. Non-Pharmacological Treatments
Cognitive Behavioral Therapy (CBT): Effective for tension and stress-related headaches.
Acupuncture: Can provide relief for chronic headaches.
Biofeedback: Helps patients control physiological functions that cause headaches.
Massage and physical therapy: Useful for muscle-tension-related headaches.
4. Prevention Strategies
Preventing headaches often involves lifestyle adjustments. Here are key strategies:
Regular Sleep: Maintain a consistent sleep schedule.
Hydration: Drink enough water throughout the day.
Healthy Diet: Avoid skipping meals and reduce consumption of trigger foods.
Exercise: Engage in regular physical activity to reduce stress and improve circulation.
Stress Management: Practice relaxation techniques such as yoga, meditation, or deep breathing exercises.
Limit Screen Time: Use blue light filters and take breaks to reduce eye strain.
5. When to See a Doctor
Consult a healthcare professional if you experience:
Sudden, severe headaches
Headaches after a head injury
Frequent headaches disrupting daily life
Neurological symptoms (blurred vision, weakness, confusion)
These could indicate a serious medical condition requiring immediate attention.
Step-by-Step Guide to Writing a Similar Article
Step 1: Choose Your Topic
Pick a health-related issue that’s common and useful to readers. For this article, we chose “Headaches.”
Step 2: Conduct Research
Use reliable sources such as:
Medical journals (PubMed)
Government websites (CDC, NIH, WHO)
Reputable health organizations (Mayo Clinic, WebMD)
Step 3: Create an Outline
Organize the content into logical sections:
Introduction
Causes and types
Triggers
Treatments
Prevention
When to see a doctor
Conclusion (optional)